Polycystic Ovary Syndrome (PCOS) is a prevalent endocrine disorder, affecting an estimated 6–12% of women of reproductive age worldwide. It is the single most common cause of anovulatory infertility—the inability to conceive due to a lack of ovulation—making it a primary concern for women and couples trying to build a family. Recognizing and managing this condition is critical, not only for achieving pregnancy but also for preventing long-term health complications.
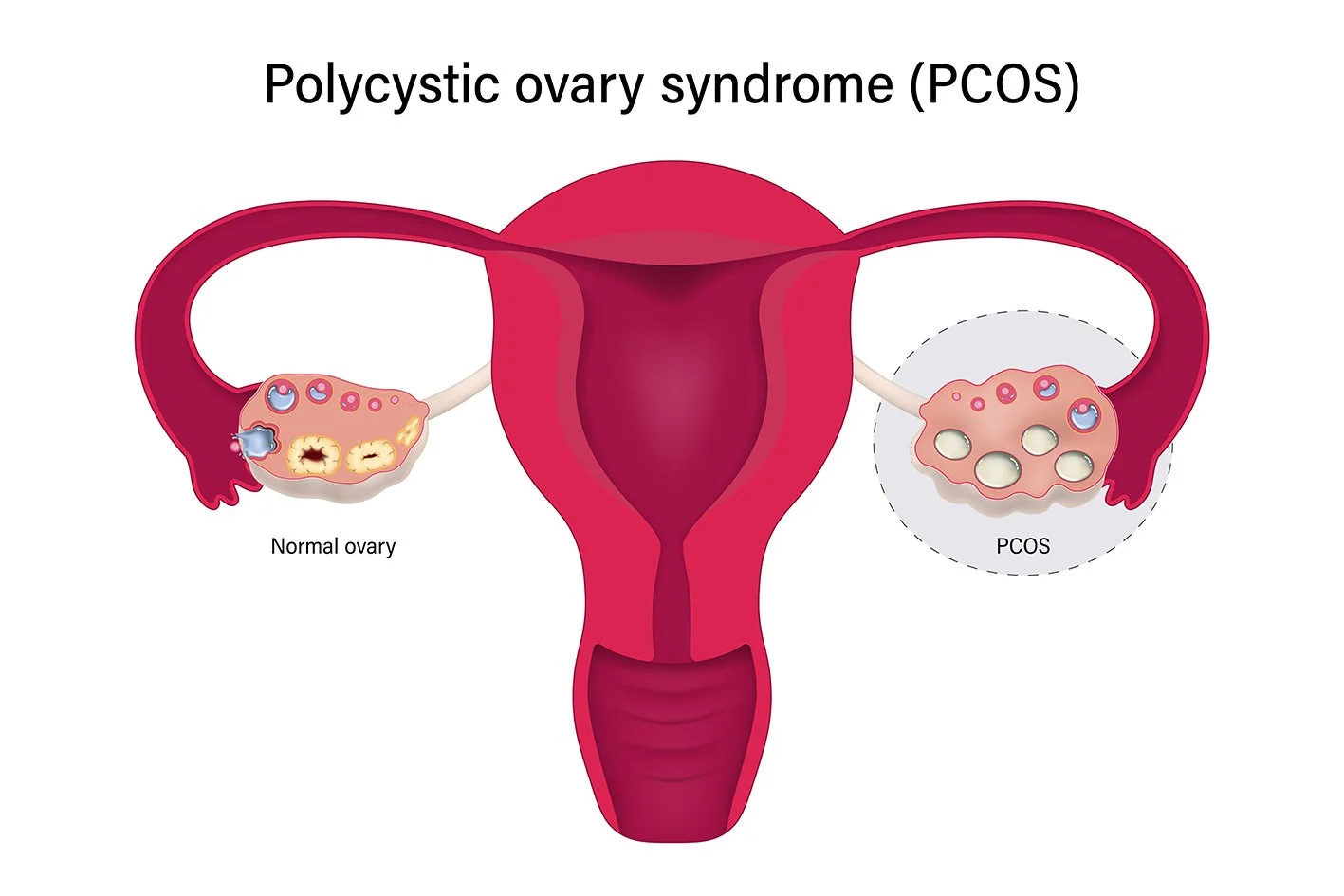
The term “polycystic” refers to the appearance of numerous small, fluid-filled sacs (follicles, not true cysts) on the ovaries, visible on an ultrasound. These follicles are underdeveloped and fail to mature and release an egg each month. However, PCOS is much more than just a problem with the ovaries; it is a complex hormonal and metabolic disorder that impacts a woman’s entire body.
The global incidence of undiagnosed PCOS is staggering, with up to 70% of affected women unaware of their condition. This delayed diagnosis often means that women only seek help when they experience difficulty conceiving, highlighting the urgent need for broader awareness and effective PCOS management strategies across the healthcare spectrum.
The Hormonal Labyrinth: Why PCOS Causes Infertility
The core issue linking PCOS and female infertility is the disruption of the normal ovulatory cycle, a process known as anovulation. This disruption stems from a hormonal cascade involving three main components:
- High Androgens (Male Hormones): Women with PCOS often produce higher-than-normal levels of androgens (like testosterone). These excess hormones interfere with the signals from the pituitary gland that normally trigger an egg to mature and be released from the ovary. Instead, the follicles stall, forming the characteristic “polycystic” appearance.
- Insulin Resistance: This is a key underlying driver in up to 70% of women with PCOS, particularly those who are overweight. Insulin Resistance causes the body to produce too much insulin. High insulin levels then signal the ovaries to produce even more androgens, exacerbating the hormonal imbalance and shutting down ovulation.
- Irregular or Absent Periods: Because eggs are not being released, the menstrual cycle becomes erratic, or ceases entirely. Without a mature egg, fertilization is impossible, directly leading to infertility. The irregularity of periods is a major sign of an underlying ovulatory disorder.
🩺 Diagnosing PCOS: Identifying the Symptoms
Diagnosing PCOS requires meeting at least two of the three criteria known as the Rotterdam Criteria, after excluding other possible causes for the symptoms:
- Oligo- or Anovulation: Infrequent (oligomenorrhea) or absent (amenorrhea) menstrual periods, indicating a lack of regular ovulation.
- Clinical or Biochemical Hyperandrogenism: Physical signs of high androgen levels (like severe acne, male-pattern hair thinning, or excess body and facial hair, known as hirsutism), or elevated androgen levels detected via blood tests.
- Polycystic Ovaries on ultrasound (12 or more follicles measuring 2–9 mm in one or both ovaries, or increased ovarian volume).
Beyond Infertility: Side Effects and Long-Term Risks
While female infertility is a critical concern, the scope of PCOS is far-reaching. The hormonal and metabolic disruptions present significant side effects and health risks:
- Weight Gain: Especially around the abdomen, which is often tied to Insulin Resistance.
- Hirsutism and Acne: Persistent, often distressing symptoms caused by high androgen levels.
- Metabolic Syndrome: Increased risk of developing Type 2 Diabetes, high cholesterol, and hypertension (high blood pressure).
- Endometrial Cancer: Due to chronic anovulation, the uterine lining (endometrium) is not regularly shed, increasing the risk of this cancer over time.
- Mental Health Challenges: Anxiety, depression, and poor body image are common side effects resulting from physical symptoms like hirsutism and difficulty with weight management.
💊 Primary Treatment Pathways for Conceiving with PCOS
The treatment approach for a woman with PCOS is highly personalized and depends entirely on her primary goal. When the goal is to overcome PCOS-related infertility and achieve pregnancy, treatment focuses on restoring regular ovulation.
1. Lifestyle Changes: The First Line of Defense
For many women, simple, sustainable lifestyle changes can significantly improve hormonal balance and may even restore ovulation naturally. Even a modest weight loss of 5-10% in women with obesity can dramatically improve fertility outcomes.
- PCOS Diet: Focus on a low-glycemic, anti-inflammatory diet. Emphasize whole grains, lean proteins, and healthy fats, while drastically reducing refined carbohydrates and sugars.
- Exercise: Moderate, regular physical activity improves insulin sensitivity and helps with weight management.
2. Medications to Induce Ovulation
When lifestyle changes are insufficient, medication is the next step to stimulate the ovaries. These drugs essentially override the hormonal imbalance to force the release of a mature egg.
- Clomiphene Citrate (Clomid): A Selective Estrogen Receptor Modulator (SERM). This is often the first-line medication, taken orally for five days early in the cycle. It works by tricking the brain into producing more Follicle-Stimulating Hormone (FSH), thereby promoting follicle growth. Uses: Primary for ovulation induction. Side Effects: Hot flashes, mood swings, risk of multiple births.
- Letrozole (Femara): An aromatase inhibitor that is now frequently preferred over Clomiphene, especially in women with PCOS. It is believed to create a more natural ovulatory environment. Uses: Highly effective for ovulation induction. Side Effects: Fatigue, dizziness, less risk of side effects on the endometrial lining than Clomiphene.
- Metformin: An insulin-sensitizing drug, commonly used for Type 2 Diabetes, is also a staple in PCOS treatment. Uses: It lowers insulin and androgen levels, which can help regulate menstrual cycles and restore ovulation. Side Effects: Gastrointestinal upset, nausea.
3. Advanced Fertility Treatments (ART)
When oral medications fail to achieve ovulation (Clomiphene resistance), or for couples with other concurrent fertility issues, Assisted Reproductive Technology (ART) becomes necessary.
- Gonadotropins and IUI (Intrauterine Insemination): Injectable hormone medications (Gonadotropins) directly stimulate the ovaries. This is a potent treatment and requires close monitoring to prevent Ovarian Hyperstimulation Syndrome (OHSS). This is often followed by IUI.
- IVF (In Vitro Fertilization): This is the most effective treatment. Ovarian stimulation is used to collect multiple eggs, which are then fertilized in a lab, and the resulting embryo is transferred to the uterus. IVF bypasses the need for the body to ovulate naturally. Uses: Highest success rates for conception. Side Effects: Ovarian hyperstimulation syndrome (OHSS) risk, emotional stress.
🌍 Global Supply and Access to PCOS Treatments
The accessibility of these essential treatments, particularly medications like Clomiphene Citrate and Metformin, varies significantly globally (excluding India). In developed healthcare markets, access is generally high, though the cost of advanced treatments like IVF remains a barrier.
However, in many parts of the world, access to timely PCOS diagnosis and treatment is hindered by a lack of specialized Reproductive Endocrinology expertise and the high cost of fertility drugs. This creates a global health disparity, where thousands of women are unable to access the help they need to manage their symptoms and achieve pregnancy. The global pharmaceutical supply chain for these products is relatively stable, with major generic and branded manufacturers ensuring widespread availability of oral medications, but the injectable Gonadotropins used in advanced ART are high-value and require strict cold-chain logistics, often making them less available in remote or less-developed regions.
📝 Conclusion: A Managed Condition
PCOS is a chronic, lifelong condition that currently has no cure, but it is highly manageable, especially when it comes to fertility. With a combination of lifestyle changes, targeted fertility drugs like Clomiphene and Letrozole, and advanced treatments such as IVF, the outlook for women with PCOS hoping to conceive is overwhelmingly positive. Early diagnosis, consistent adherence to a management plan, and focusing on improving underlying Insulin Resistance are the most effective steps a woman can take to manage the disorder’s side effects, mitigate long-term health risks, and ultimately, achieve a healthy pregnancy.
Referennces:-
World Health Organization (WHO): Polycystic Ovary Syndrome
The Lancet: Review on the long-term health consequences of PCOS
- https://academic.oup.com/humupd/article/12/6/673/625165 (Link to a major meta-analysis on long-term pregnancy and health complications.)
Cochrane Review: Efficacy of Clomiphene Citrate versus Letrozole for ovulation induction in PCOS
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6494577/ (Link to the PubMed Central full text of the Cochrane Review on Letrozole vs. Clomiphene Citrate.)
American Society for Reproductive Medicine (ASRM): Guidelines on the diagnosis and management of PCOS
- https://www.monash.edu/__data/assets/pdf_file/0004/1412644/PCOS_Evidence-Based-Guidelines_20181009.pdf (Link to the comprehensive International Evidence-Based Guidelines co-sponsored by ASRM.)
The National Institutes of Health (NIH): Study on the role of Metformin in improving insulin sensitivity in PCOS patients
- https://academic.oup.com/jcem/article-abstract/99/5/1870/2537672 (Link to a study on Metformin and glucose effectiveness in PCOS, published in an Endocrine Society journal with NIH funding.)






Add comment